What Data Fragmentation Means for the Patient?
What Data Fragmentation Means for the Patient?
Do you know what data fragmentation means for the patient? Data flow and management are more important than ever. However, among the industry’s biggest challenges is healthcare data fragmentation – where patient data is fragmented across systems, providers and organizations.
A McKinsey study found that 20-25% of US healthcare expenditure, more or less $1 trillion, is wasted. And 50-75% of this waste might be eliminated by better data utilization – potentially saving the U.S. healthcare system between $500 billion and $750 billion.
This data fragmentation is costly, impedes efficient care delivery, and adversely impacts the patient experience.
Let’s explore what healthcare data fragmentation is, why it happens, and how it affects patients.
Understanding Healthcare Data Fragmentation
Healthcare data fragmentation is the dispersal of a patient’s medical information across systems, facilities, and databases. A patient might be seen by a primary care physician, specialists, labs, imaging centers, and hospitals that maintain their own electronic health record (EHR) system.
These systems often do not communicate effectively, so vital health data remains locked up in silos and unavailable when most needed.
The problem is further exacerbated by a lack of standardization in health IT systems. Different EHR platforms may store and format data differently, limiting interoperability – a seamless exchange of information. Efforts such as the adoption of FHIR (Fast Healthcare Interoperability Resources) standards have reduced data fragmentation, but it is still a systemic problem.
Causes of Health Data Fragmentation
Disparate Systems and Providers
Healthcare organizations often adopt EHR systems independently, leading to poor coordination. A cardiology doctor might use one system, while the individual’s primary care doctor uses another, with little or no overlap.
Geographic Barriers
When patients move or seek care in another city or state, their medical records may not follow them because of regional health information exchange (HIE) limitations. To continue care without any disruption, patients typically have to manually request records to be sent to their new providers.
Inconsistent Patient Portals
Many providers offer patient portals, but these are tied to specific practices or systems. Patients may have to log into several portals to view their full medical history.
Policy and Privacy Constraints
Regulative frameworks such as HIPAA place data security and privacy first, sometimes at the expense of easy data sharing. Although well intended, these regulations create bottlenecks in information flow.
How Data Fragmentation Affects Patients
Delayed or Inaccurate Diagnoses
Healthcare providers that don’t have access to an individual’s complete medical history risk making choices based on out-of-date or incomplete information. This can cause misdiagnoses, redundant tests, or unnecessary treatments.
Higher Costs
Fragmentation often leads to duplicated diagnostic tests, imaging or procedures, increasing healthcare costs for patients and the system as a whole.
Poor Care Coordination
Poor care coordination is most evident in chronic disease patients who see several specialists frequently. Without a unified view of the patient’s data, providers may not collaborate effectively, resulting in inconsistent treatment plans.
Patient Frustration
Numerous patients must manually consolidate their medical records, a time-consuming and error-prone process. This barrier to access erodes trust in the healthcare system and adds stress during already difficult times.
Lower Health Outcomes
Fragmented data may limit preventive care and long-term management of certain conditions, leading to poorer health outcomes. For example, a missed lab result or an overlooked allergy can have serious (sometimes fatal) consequences.
The Future of Healthcare: Breaking Down Silos
Healthcare organizations are realizing the need to break down data silos. Policy changes, technological advances, and patient advocacy drive a move toward greater interoperability and centralized data access.
For patients, this means fewer delays, lower costs, and better care quality. Instead, providers become better informed and less likely to make errors, improving outcomes.
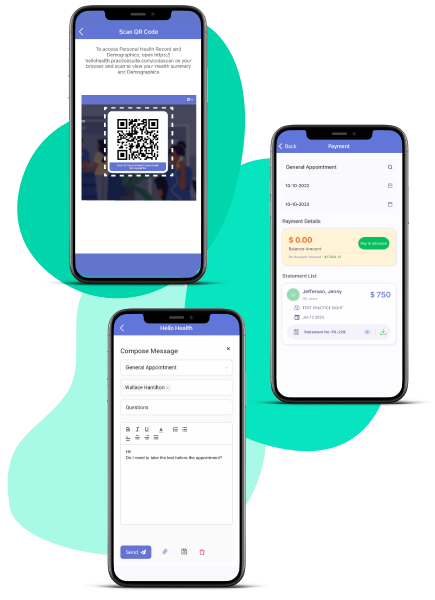
Patient-centric solutions like HelloHealth offer a blueprint for addressing data fragmentation as we move forward. By prioritizing accessibility and user-friendly tools, healthcare providers can finally transcend their fragmented past and deliver the seamless experience patients deserve.
A Path Forward
Healthcare data fragmentation remains a persistent problem with serious implications for patients. However, there is a way forward with the rise of centralized digital solutions.
Tools like HelloHealth’s app bring everything together: patient records, appointments, provider communications and prescription management – all in one place.
Adopting innovation and focusing on connectivity could redefine the healthcare experience – where providers and patients benefit equally from access to the information they require.